Tenwek has been a unique experience for me this year. I have
struggled to understand why it is so. Since the Ob-Gyn department now has three
levels of our Ob-Gyn Residency in place, a lot of the minute-by-minute
decisions are made by them. I now serve more as a consultant/staff person
overseeing their decision-making and growing surgical skills. I rarely need to
“scrub-in” to guide them through a gynecologic or obstetrical procedure, even
though I am in the room.
I already have great respect for the nurse midwives who
manage actively laboring patients. However, for the 40-50% of our patients who
need cesarean sections, I will participate in the decision making by the
clinical and medical officers (PA and Medicine interns)and the residents. I cannot
decide if I am like a “fly on the wall” or some “guardian angel” viewing from
above. Both are quite foreign to me.
This has allowed me to process patients and their clinical
situations on a bigger scale. I miss the intimate relationships I had developed
with patients in the past. But I appreciate more the challenges these patients bring
to their primary caregivers from this new perspective.
I see the trust that the
patient/mother has for them as she deals with a pregnancy loss-either early or
later in gestation. I see the fear of life-threatening diagnoses to herself and
her baby. Examples include severe hypertension, uncontrolled diabetes, an
enormous number of serious blood clots and strokes, advanced cervical and other gyn cancers, heart failure (in a 17 year
old after delivering a premature baby that didn’t survive), overwhelming
infections and an unbelievably high number of twin pregnancies (1/20
pregnancies are twins in Kenya), and on…and on….
It takes a special patience to try
to educate our patients about their diagnoses. Most patients are poorly educated,
and medical jargon has to be translated very simply. I see the interns and
residents sitting for long periods with
the patients who do not even know what questions to ask.
I have seen vast improvements over
the past 12 years in the resources available to treat patients. The Blood Bank is
not as dependent on missionaries and visiting staff to donate blood as in the
past. It is customary for surgical patients to have family members donate almost
without exception, and if un-used, the blood can be used for other patients
(which is better than in the US!).
We all need success stories. Here is
mine (ours!). (JC) is a 25-year-old 8-month pregnant woman who was in a
motorcycle accident. She underwent an emergency cesarean delivery at another
facility, but the baby was stillborn. 5 days later she was transferred to
Tenwek Hospital with an overwhelming infection. We did an exploratory surgery only
to find a tear in her small bowel! This was directly related to the blunt
trauma to her abdomen sustained during the accident! General surgeons were
called in to repair it and to take over the care of the patient. She has now had seven (7!!) more surgeries to ‘clean out’
the problems resulting from the infection and damage to the bowel. We thank God
that she will almost assuredly survive. She will need prayerful care as she
struggles with the loss of her baby, AND the physical demands on her body. We
strongly lean on “We Treat….Jesus Heals.”
We all need time to escape, recover,
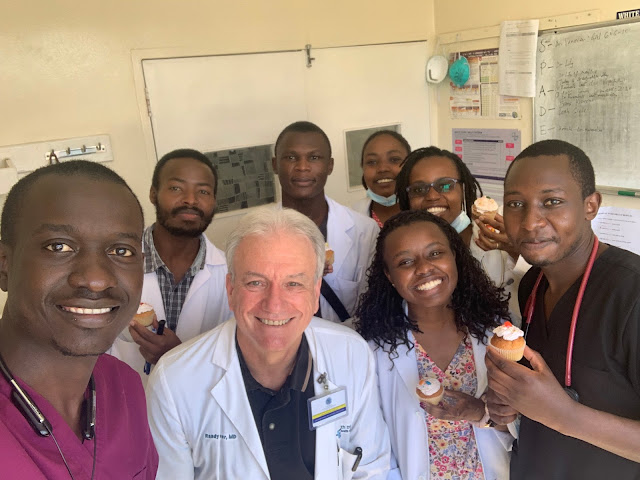
and be reminded of God’s sovereignty. This weekend Randy, Madison (U.S. ObGyn
resident visiting here with us) and I went of several safari rides. God’s
creativity was on full display with the variety of animals we saw and the
beauty of His physical world. We were humbled. We thank God for allowing us to be
here and to experience the broad array of emotions that we always experience in
Kenya and at Tenwek specifically.
I thank you for sharing this
experience with me/us.
Love, Marilyn (Randy and Madison)
 |
| Sunset on the Mara... |